What would you do if someone put a gun to your head? Realistically – you’d panic. And you shouldn’t feel bad about that reaction, because the fight-or-flight response is a pretty useful evolutionary tool to keep you alive. But, hypothetically, what if someone would put a gun to your head everyday? Now that’s another story.
What would you do if someone put a gun to your head? Realistically – you’d panic. And you shouldn’t feel bad about that reaction, because the fight-or-flight response is a pretty useful evolutionary tool to keep you alive. But, hypothetically, what if someone would put a gun to your head everyday? Now that’s another story.
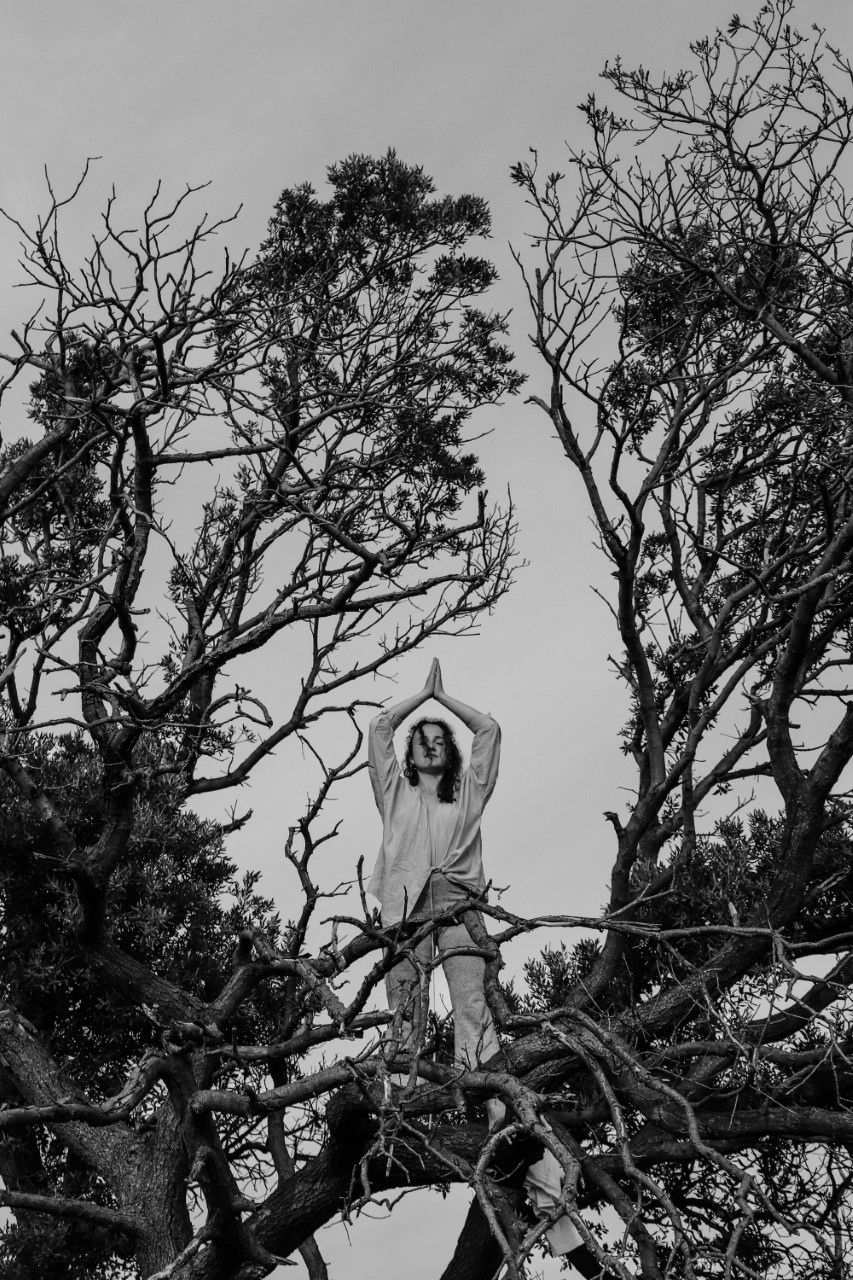
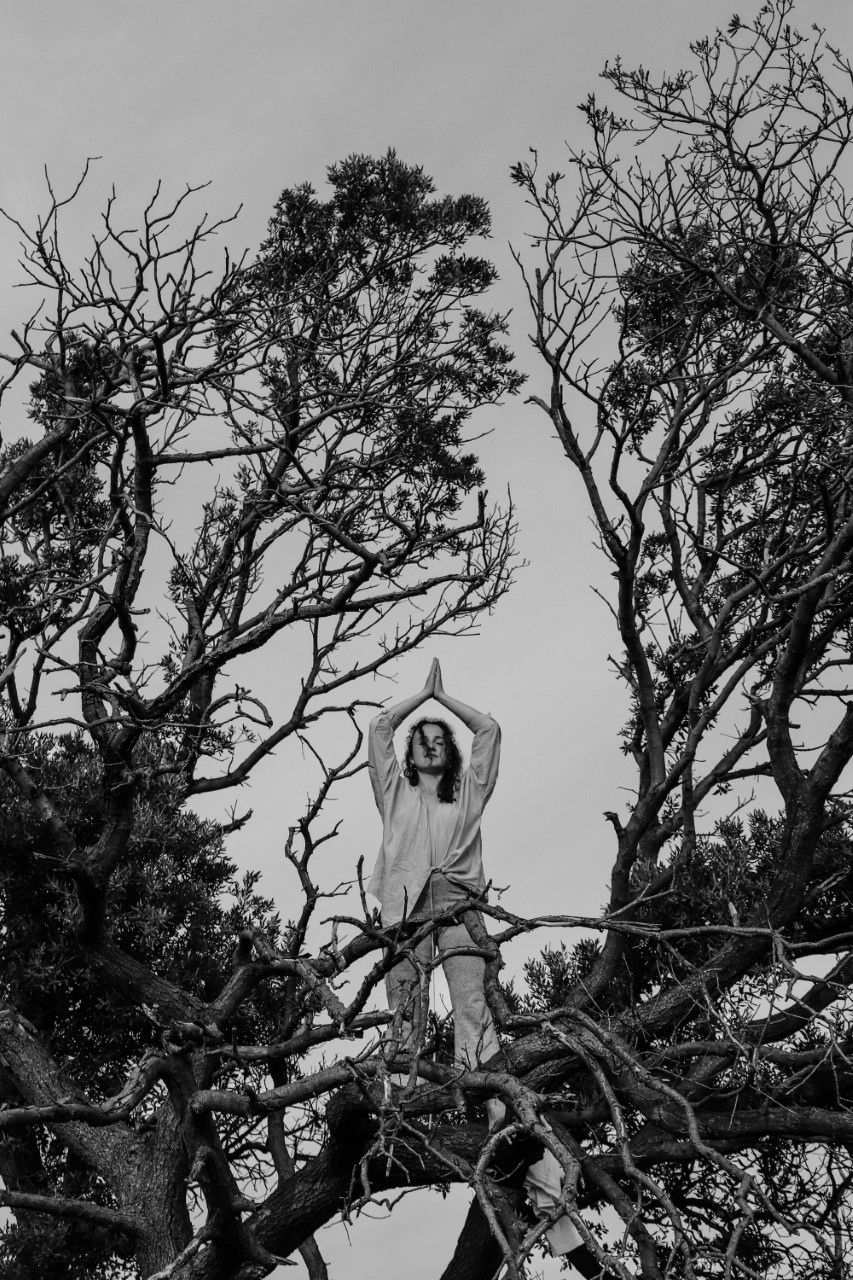
Photo by Pika Ivana Kostanjšek
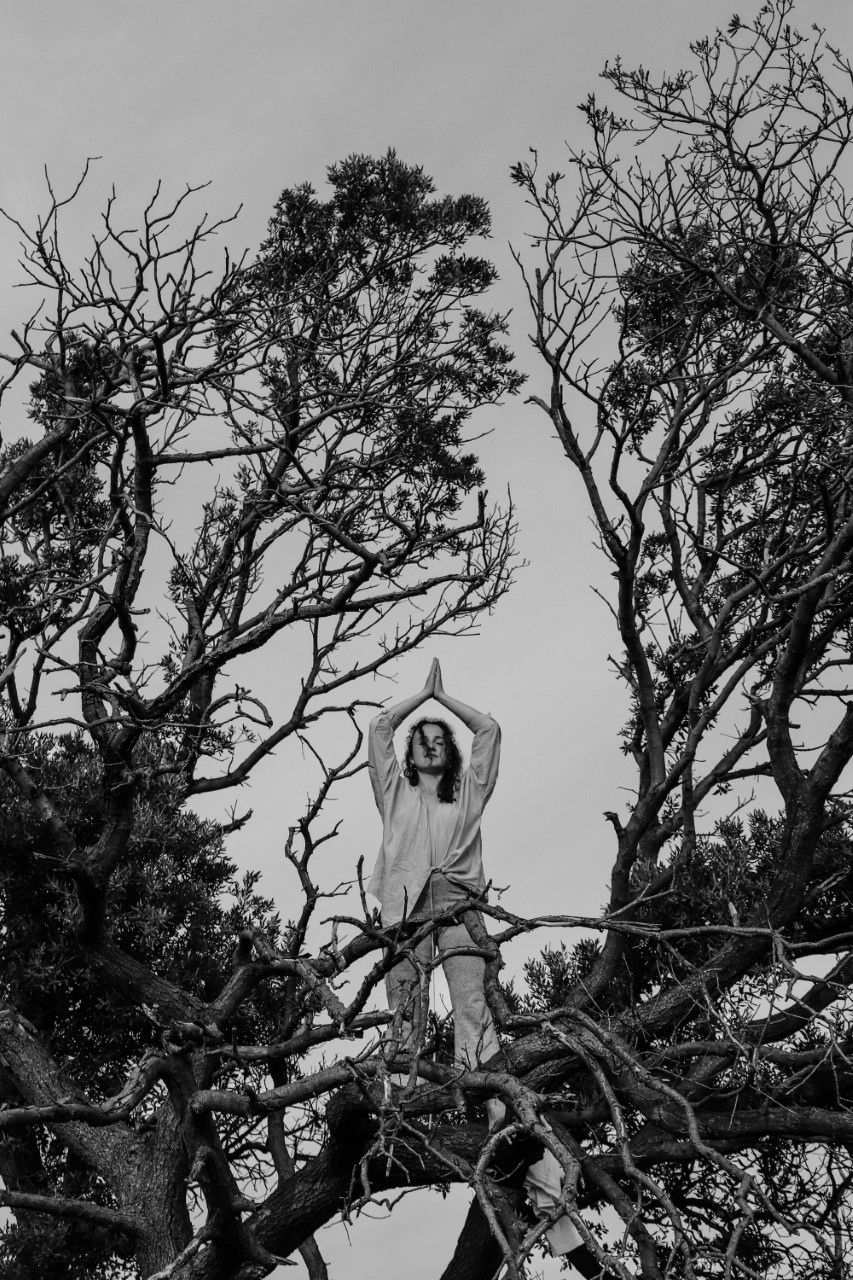
Photo by Pika Ivana Kostanjšek
Unless you’re really unlucky, you probably haven’t lived through the experience of being held at gunpoint everyday. For some people though, the adrenaline response your body would elicit to save your life, is ever present – and if a fire alarm keeps ringing, even with no fire, then it renders the alarm quite useless. The analogy of being under constant attack, be it a pointed gun or tiger chasing you, is common in describing the daily experience of living with various anxiety or trauma disorders, such as Generalized Anxiety Disorder (GAD) or Post Traumatic Stress Disorder (PTSD).
One of the most common treatments for such disorders is Cognitive Behavioral Therapy (CBT), and for good reason. Our knowledge through many studies suggests it is a well-accepted and effective treatment for anxiety and trauma disorders, though individual effectiveness naturally varies (Otte, 2011). However, no treatment is perfect, and CBT is no stranger to that fate. Plenty of studies concerning CBT focus on participants who have not before experienced similar therapies, which while obvious from the standpoint of experimental research, poses a problem that has become overlooked despite being plain to see – what happens to the people who didn’t get better under CBT treatment? This question is important to answer, because the response rate for CBT treatment in GAD is around 50%, which – while high – leaves a whole lot of patients requiring further treatment (Loreinc et al, 2015).
If the “gold standard” of treatment didn’t work for you, it must feel like a hopeless place to be in. I feel pretty confident in this statement, because I was in the same situation. After years of therapy, my own condition seemingly got worse instead of better, and no one could provide an answer as to why, or what could help instead. That is, until my last therapist stumbled upon a little green book about somatic therapy exercises, and introduced me to something that was able to restore hope.
“If the “gold standard” of treatment didn’t work for you, it must feel like a hopeless place to be in.”
Body-oriented or somatic therapies are therapeutic treatments which focus on the body, standing upon the idea that mental problems may arise in the mind, but cannot necessarily be treated by targeting thought alone. One of the most well known and first such treatments is Somatic Experiencing, a method coined by Peter A. Levine (1997). In his book, “Waking the Tiger”, he describes his work with patients and uses the analogy of living as if always being chased by a tiger quite frequently (Levine & Frederick, 1997). To understand why body-oriented therapies can be effective and useful, a quick neurobiology lesson may prove beneficial.
The nervous system has two divisions, sympathetic and parasympathetic. The sympathetic division doesn’t live up to its name, as it is the one responsible for the fight-or-flight response in the face of perceived threat. When the danger passes, the parasympathetic division is responsible for bringing the body back to its relaxed, calm state (McCorry, 2007). Furthermore, a system called the HPA axis produces cortisol, the primary stress hormone (Sheng et al, 2021). In equilibrium, these functions of the body help to keep you alive by alerting you to danger and having other regulatory purposes.
However, in the case of those living with an anxiety or trauma disorder, these systems become disrupted. Chronic stress can lead to the constant activation of the HPA axis, causing heightened cortisol levels, which poses serious health problems (Staufenbiel et al, 2013). In the case of the nervous system, even when the big scary wolf turns out to be a bunny rabbit, the sympathetic division may not get the memo that it’s time to give their brother a turn to play. The parasympathetic division rarely activating means the body doesn’t regulate after threat efficiently, making it more vulnerable to future threat.
Healing the disruption of these systems is exactly the focus of body-oriented therapies. The idea is that, if the mind and body work together, then by focusing on rebalancing the nervous system, one can stop living as if they were constantly under threat. These approaches use a variety of strategies to achieve this. A fundamental concept relates to breathwork – different breathing exercises are incorporated into treatment in order to reestablish an equilibrium of the nervous system. While many therapies already use breathing exercises, they tend to focus on using them as tools for calming down after triggering situations. Somatic therapies on the other hand, incorporate these exercises into the daily routine, and patients are encouraged to practice them as often as possible, even when they feel perfectly fine.
Other than a multitude of approaches to breathwork, body-oriented therapies also consist of gentle movement, such as yoga or walking, as opposed to strenuous exercise (Khalsa et al, 2014). Furthermore, multiple techniques are used to help patients feel more grounded in their bodies. One of the best things about this approach of therapy is that it is highly adjustable to individual patients, and through the guidance of a therapist, personalized strategies can be developed to aid in returning to balance.
“In the case of the nervous system, even when the big scary wolf turns out to be a bunny rabbit, the sympathetic division may not get the memo that it's time to give their brother a turn to play.”
Somatic therapies are still a rather new area of treatment, and as such, many studies still need to be done, although so far the data gathered has been quite promising. Such therapies aid in building resilience, meaning future events are less likely to have long lasting traumatic effects, and allow for conscious response to them as opposed to through the use of automatic anxiety responses. They help to create a safe internal environment for processing emotions without triggering panic attacks for instance, and are suited for targeting the somatic symptoms of mental illness (Van Der Kolk, 2014).
Granted, all things have their drawbacks. These approaches require a lot of patience to see long term results, and are rarely sufficient as a standalone treatment. Nevertheless, for those who were failed by CBT, or have conditions more chronic than most studies on the effectiveness of talk therapies would consider, somatic therapies may be a lifeline.
Incorporating these approaches alongside existing treatments has the potential to deliver fantastic results, and allows us to finally begin to formulate an answer to the question of what happens to people who don’t get better from CBT. And if the answer still isn’t complete, we keep looking, bringing us a step closer to it than before.
Turns out, even if your faulty fire alarm keeps ringing, there are ways you can fix it. An alarm that alerts to danger, but is otherwise silent, is bliss. So let’s switch out the batteries – it is due time to be reminded how living in peace feels like.
References
– Khalsa, M. K., Greiner-Ferris, J. M., Hofmann, S. G., & Khalsa, S. B. S. (2014). Yoga-Enhanced Cognitive Behavioural Therapy (Y-CBT) for Anxiety Management: A Pilot Study. Clinical Psychology &Amp; Psychotherapy, 22(4), 364–371. https://doi.org/10.1002/cpp.1902
– Levine, P. A., PhD, & Frederick, A. (1997). Waking the Tiger: Healing Trauma: The Innate Capacity to Transform Overwhelming Experiences. Adfo Books.
– Loerinc, A. G., Meuret, A. E., Twohig, M. P., Rosenfield, D., Bluett, E. J., & Craske, M. G. (2015). Response rates for CBT for anxiety disorders: Need for standardized criteria. Clinical Psychology Review, 42, 72–82. https://doi.org/10.1016/j.cpr.2015.08.004
– McCorry, L. K. (2007). Physiology of the Autonomic Nervous System. American Journal of Pharmaceutical Education, 71(4), 78. https://doi.org/10.5688/aj710478
– Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues in Clinical Neuroscience, 13(4), 413–421. https://doi.org/10.31887/dcns.2011.13.4/cotte
– Sheng, J. A., Bales, N. J., Myers, S. A., Bautista, A. I., Roueinfar, M., Hale, T. M., & Handa, R. J. (2021). The Hypothalamic-Pituitary-Adrenal Axis: Development, Programming Actions of Hormones, and Maternal-Fetal Interactions. Frontiers in Behavioral Neuroscience, 14. https://doi.org/10.3389/fnbeh.2020.601939
– Staufenbiel, S. M., Penninx, B. W., Spijker, A. T., Elzinga, B. M., & Van Rossum, E. F. (2013). Hair cortisol, stress exposure, and mental health in humans: A systematic review. Psychoneuroendocrinology, 38(8), 1220–1235. https://doi.org/10.1016/j.psyneuen.2012.11.015
– Van der Kolk, B. (2015). The Body Keeps the Score: Mind, Brain and Body in the Transformation of Trauma. Adfo Books.
Unless you’re really unlucky, you probably haven’t lived through the experience of being held at gunpoint everyday. For some people though, the adrenaline response your body would elicit to save your life, is ever present – and if a fire alarm keeps ringing, even with no fire, then it renders the alarm quite useless. The analogy of being under constant attack, be it a pointed gun or tiger chasing you, is common in describing the daily experience of living with various anxiety or trauma disorders, such as Generalized Anxiety Disorder (GAD) or Post Traumatic Stress Disorder (PTSD).
One of the most common treatments for such disorders is Cognitive Behavioral Therapy (CBT), and for good reason. Our knowledge through many studies suggests it is a well-accepted and effective treatment for anxiety and trauma disorders, though individual effectiveness naturally varies (Otte, 2011). However, no treatment is perfect, and CBT is no stranger to that fate. Plenty of studies concerning CBT focus on participants who have not before experienced similar therapies, which while obvious from the standpoint of experimental research, poses a problem that has become overlooked despite being plain to see – what happens to the people who didn’t get better under CBT treatment? This question is important to answer, because the response rate for CBT treatment in GAD is around 50%, which – while high – leaves a whole lot of patients requiring further treatment (Loreinc et al, 2015).
If the “gold standard” of treatment didn’t work for you, it must feel like a hopeless place to be in. I feel pretty confident in this statement, because I was in the same situation. After years of therapy, my own condition seemingly got worse instead of better, and no one could provide an answer as to why, or what could help instead. That is, until my last therapist stumbled upon a little green book about somatic therapy exercises, and introduced me to something that was able to restore hope.
“If the “gold standard” of treatment didn’t work for you, it must feel like a hopeless place to be in.”
Body-oriented or somatic therapies are therapeutic treatments which focus on the body, standing upon the idea that mental problems may arise in the mind, but cannot necessarily be treated by targeting thought alone. One of the most well known and first such treatments is Somatic Experiencing, a method coined by Peter A. Levine (1997). In his book, “Waking the Tiger”, he describes his work with patients and uses the analogy of living as if always being chased by a tiger quite frequently (Levine & Frederick, 1997). To understand why body-oriented therapies can be effective and useful, a quick neurobiology lesson may prove beneficial.
The nervous system has two divisions, sympathetic and parasympathetic. The sympathetic division doesn’t live up to its name, as it is the one responsible for the fight-or-flight response in the face of perceived threat. When the danger passes, the parasympathetic division is responsible for bringing the body back to its relaxed, calm state (McCorry, 2007). Furthermore, a system called the HPA axis produces cortisol, the primary stress hormone (Sheng et al, 2021). In equilibrium, these functions of the body help to keep you alive by alerting you to danger and having other regulatory purposes.
However, in the case of those living with an anxiety or trauma disorder, these systems become disrupted. Chronic stress can lead to the constant activation of the HPA axis, causing heightened cortisol levels, which poses serious health problems (Staufenbiel et al, 2013). In the case of the nervous system, even when the big scary wolf turns out to be a bunny rabbit, the sympathetic division may not get the memo that it’s time to give their brother a turn to play. The parasympathetic division rarely activating means the body doesn’t regulate after threat efficiently, making it more vulnerable to future threat.
Healing the disruption of these systems is exactly the focus of body-oriented therapies. The idea is that, if the mind and body work together, then by focusing on rebalancing the nervous system, one can stop living as if they were constantly under threat. These approaches use a variety of strategies to achieve this. A fundamental concept relates to breathwork – different breathing exercises are incorporated into treatment in order to reestablish an equilibrium of the nervous system. While many therapies already use breathing exercises, they tend to focus on using them as tools for calming down after triggering situations. Somatic therapies on the other hand, incorporate these exercises into the daily routine, and patients are encouraged to practice them as often as possible, even when they feel perfectly fine.
Other than a multitude of approaches to breathwork, body-oriented therapies also consist of gentle movement, such as yoga or walking, as opposed to strenuous exercise (Khalsa et al, 2014). Furthermore, multiple techniques are used to help patients feel more grounded in their bodies. One of the best things about this approach of therapy is that it is highly adjustable to individual patients, and through the guidance of a therapist, personalized strategies can be developed to aid in returning to balance.
“In the case of the nervous system, even when the big scary wolf turns out to be a bunny rabbit, the sympathetic division may not get the memo that it's time to give their brother a turn to play.”
Somatic therapies are still a rather new area of treatment, and as such, many studies still need to be done, although so far the data gathered has been quite promising. Such therapies aid in building resilience, meaning future events are less likely to have long lasting traumatic effects, and allow for conscious response to them as opposed to through the use of automatic anxiety responses. They help to create a safe internal environment for processing emotions without triggering panic attacks for instance, and are suited for targeting the somatic symptoms of mental illness (Van Der Kolk, 2014).
Granted, all things have their drawbacks. These approaches require a lot of patience to see long term results, and are rarely sufficient as a standalone treatment. Nevertheless, for those who were failed by CBT, or have conditions more chronic than most studies on the effectiveness of talk therapies would consider, somatic therapies may be a lifeline.
Incorporating these approaches alongside existing treatments has the potential to deliver fantastic results, and allows us to finally begin to formulate an answer to the question of what happens to people who don’t get better from CBT. And if the answer still isn’t complete, we keep looking, bringing us a step closer to it than before.
Turns out, even if your faulty fire alarm keeps ringing, there are ways you can fix it. An alarm that alerts to danger, but is otherwise silent, is bliss. So let’s switch out the batteries – it is due time to be reminded how living in peace feels like.